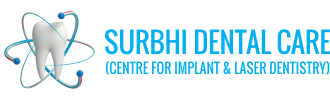
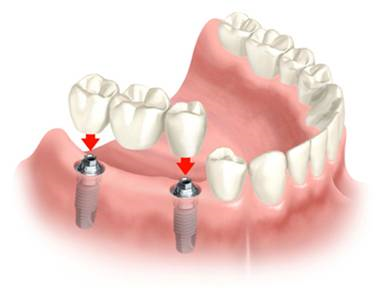
A dental implant is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor. The basis for modern dental implants is a biologic process called osseointegration, in which materials such as titanium form an intimate bond to bone. The implant fixture is first placed so that it is likely to osseointegrate, then a dental prosthetic is added. A variable amount of healing time is required for osseointegration before either the dental prosthetic (a tooth, bridge or denture) is attached to the implant or an abutment is placed which will hold a dental prosthetic.
Success or failure of implants depends on the health of the person receiving the treatment, drugs which affect the chances of osseointegration and the health of the tissues in the mouth. The amount of stress that will be put on the implant and fixture during normal function is also evaluated. The prerequisites for long-term success of osseointegrated dental implants are healthy bone and gingiva. Since both can atrophy after tooth extraction, pre-prosthetic procedures such as sinus lifts or gingival grafts are sometimes required to recreate ideal bone and gingiva.
The final prosthetic can be either fixed, where a person cannot remove the denture or teeth from their mouth, or removable, where they can remove the prosthetic. In each case an abutment is attached to the implant fixture. Where the prosthetic is fixed, the crown, bridge or denture is fixed to the abutment either with lag screws or with dental cement. Where the prosthetic is removable, a corresponding adapter is placed in the prosthetic so that the two pieces can be secured together.

General considerations
Planning for dental implants focuses on the general health condition of the patient, the local health condition of the mucous membranes and the jaws and the shape, size, and position of the bones of the jaws, adjacent and opposing teeth. There are few health conditions that absolutely preclude placing implants although there are certain conditions that can increase the risk of failure. Long-term steroid use, osteoporosis and other diseases that affect the bones can increase the risk of early failure of implants.
The long-term success of implants is determined, in part, by the forces they have to support. As implants have no periodontal ligament, there is no sensation of pressure when biting so the forces created are higher. To offset this, the location of implants must distribute forces evenly across the prosthetics they support. Concentrated forces can result in fracture of the bridgework, implant components, or loss of bone adjacent the implant. The ultimate location of implants is based on both biologic (bone type, vital structures, health) and mechanical factors. Implants placed in thicker, stronger bone like that found in the front part of the bottom jaw have lower failure rates than implants placed in lower density bone, such as the back part of the upper jaw. People who grind their teeth also increase the force on implants and increase the likelihood of failures
Placing the implant
Most implant systems have five basic steps for placement of each implant:
- Soft tissue reflection: An incision is made over the crest of bone, splitting the thicker attached gingiva roughly in half so that the final implant will have a thick band of tissue around it. The edges of tissue, each referred to as a flap are pushed back to expose the bone. Flapless surgery is an alternate technique, where a small punch of tissue (the diameter of the implant) is removed for implant placement rather than raising flaps.
- Drilling at high speed: After reflecting the soft tissue, and using a surgical guide or stent as necessary, pilot holes are placed with precision drills at highly regulated speed to prevent burning or pressure necrosis of the bone.
- Drilling at low speed: The pilot hole is expanded by using progressively wider drills (typically between three and seven successive drilling steps, depending on implant width and length). Care is taken not to damage the osteoblast or bone cells by overheating. A cooling saline or water spray keeps the temperature low.
- Placement of the implant: The implant screw is placed and can be self-tapping otherwise the prepared site is tapped with an implant analog. It is then screwed into place with a torque controlled wrench at a precise torque so as not to overload the surrounding bone (overloaded bone can die, a condition called osteonecrosis, which may lead to failure of the implant to fully integrate or bond with the jawbone).
- Tissue adaptation: The gingiva is adapted around the entire implant to provide a thick band of healthy tissue around the healing abutment. In contrast, an implant can be "buried", where the top of the implant is sealed with a cover screw and the tissue is closed to completely cover it. A second procedure would then be required to uncover the implant at a later date.

Timing of implants after extraction of teeth
There are different approaches to placement dental implants after tooth extraction.[22] The approaches are:
- Immediate post-extraction implant placement.
- Delayed immediate post-extraction implant placement (two weeks to three months after extraction).
- Late implantation (three months or more after tooth extraction).
There are also various options for when to attach teeth to dental implant classified into:
- Immediate loading procedure.
- Early loading (one week to twelve weeks).
- Delayed loading (over three months)
- Healing time
- For an implant to become permanently stable, the body must grow bone to the surface of the implant (osseointegration). Based on this biologic process, it was thought that loading an implant during the osseointegration period would result in movement that would prevent osseointegration, and thus increase implant failure rates. As a result, three to six months of integrating time (depending on various factors) was allowed before placing the teeth on implants (restoring them).
- However, later research suggests that the initial stability of the implant in bone is a more important determinant of success of implant integration, rather than a certain period of healing time. As a result, the time allowed to heal is typically based on the density of bone the implant is placed in and the number of implants splinted together, rather than a uniform amount of time. When implants can withstand high torque (35 Ncm) and are splinted to other implants, there are no meaningful differences in long-term implant survival or bone loss between implants loaded immediately, at three months, or at six months. The corollary is that single implants, even in solid bone, require a period of no-load to minimize the risk of initial failure.
Soft tissue reconstruction
The gingiva surrounding a tooth has a 2–3 mm band of bright pink, very strong attached mucosa, then a darker, larger area of unattached mucosa that fold into the cheeks. When replacing a tooth with an implant, a band of strong, attached gingiva is needed to keep the implant healthy in the long-term. This is especially important with implants because the blood supply is more precarious in the gingiva surrounding an implant, and is theoretically more susceptible to injury because of a longer attachment to the implant than on a tooth (a longer biologic width).
When an adequate band of attached tissue is absent, it can be recreated with a soft tissue graft. There are four methods that can be used to transplant soft tissue. A roll of tissue adjacent to an implant can be moved towards the lip, gingiva from the palate can be transplanted, deeper connective tissue from the palate can be transplanted or, when a larger piece of tissue is needed, a finger of tissue based on a blood vessel in the palate can be repositioned to the area.
Additionally, for an implant to look esthetic, a band of full, plump gingiva is needed to fill in the space on either side of implant. The most common soft tissue complication is called a black-triangle, where the papilla (the small triangular piece of tissue between two teeth) shrinks back and leaves a triangular void between the implant and the adjacent teeth. Dentists can only expect 2–4 mm of papilla height over the underlying bone. A black triangle can be expected if the distance between where the teeth touch and bone is any greater.
The prosthetic phase begins once the implant is well integrated (or has a reasonable assurance that it will integrate) and an abutment is in place to bring it through the mucosa. Even in the event of early loading (less than 3 months), many practitioners will place temporary teeth until osseointegration is confirmed. The prosthetic phase of restoring an implant requires an equal amount of technical expertise as the surgical because of the biomechanical considerations, especially when multiple teeth are to be restored. The dentist will work to restore the vertical dimension of occlusion, the esthetics of the smile, and the structural integrity of the teeth to evenly distribute the forces of the implants.

Prosthetic procedures for single teeth, bridges and fixed dentures
An abutment is selected depending on the application. In many single crown and fixed partial denture scenarios (bridgework), custom abutments are used. An impression of the top of the implant is made with the adjacent teeth and gingiva. A dental lab then simultaneously fabricates an abutment and crown. The abutment is seated on the implant, a screw passes through the abutment to secure it to an internal thread on the implant. There are variations on this, such as when the abutment and implant body are one piece or when a stock abutment is used. Custom abutments can be made by hand, as a cast metal piece or custom milled from metal or zirconia, all of which have similar success rates.
The platform between the implant and the abutment can be flat (buttress) or conical fit. In conical fit abutments, the collar of the abutment sits inside the implant which allows a stronger junction between implant and abutment and a better seal against bacteria into the implant body. To improve the gingival seal around the abutment collar, a narrowed collar on the abutment is used, referred to as platform switching. The combination of conical fits and platform switching gives marginally better long term periodontal conditions compared to flat-top abutments.
Regardless of the abutment material or technique, an impression of the abutment is then taken and a crown secured to the abutment with dental cement. Another variation on abutment/crown model is when the crown and abutment are one piece and the lag-screw traverses both to secure the one-piece structure to the internal thread on the implant. There does not appear to be any benefit, in terms of success, for cement versus screw-retained prosthetics, although the latter is believed to be easier to maintain (and change when the prosthetic fractures) and the former offers high esthetic performance.
Prosthetic procedures for removable dentures
When a removable denture is worn, retainers to hold the denture in place can be either custom made or stock abutments. When custom retainers are used, four or more implant fixtures are placed and an impression of the implants is taken and a dental lab creates a custom metal bar with attachments to hold the denture in place. Significant retention can be created with multiple attachments and the use of semi-precision attachments (such as a small diameter pin that pushes through the denture and into the bar) which allows for little or no movement in the denture, but it remains removable. However, the same four implants angled in such a way to distribute occlusal forces may be able to safely hold a fixed denture in place with comparable costs and number of procedures giving the denture wearer a fixed solution.
Alternatively, stock abutments are used to retain dentures using a male-adapter attached to the implant and a female adapter in the denture. Two common types of adapters are the ball-and-socket style retainer and the button-style adapter.
These types of stock abutments allow movement of the denture, but enough retention to improve the quality of life for denture wearers, compared to conventional dentures. Regardless of the type of adapter, the female portion of the adapter that is housed in the denture will require periodic replacement, however the number and adapter type does not seem to affect patient satisfaction with the prosthetic for various removable alternatives.

Maintenance
After placement, implants need to be cleaned (similar to natural teeth) with a Teflon instrument to remove any plaque. Because of the more precarious blood supply to the gingiva, care should be taken with dental floss. Implants will lose bone at a rate similar to natural teeth in the mouth (e.g. if someone suffers from periodontal disease, an implant can be affected by a similar disorder) but will otherwise last. The porcelain on crowns should be expected to discolour, fracture or require repair approximately every ten years, although there is significant variation in the service life of dental crowns based on the position in the mouth, the forces being applied from opposing teeth and the restoration material. Where implants are used to retain a complete denture, depending on the type of attachment, connections need to be changed or refreshed every one to two years. A powered irrigator may also be useful for cleaning around implants.